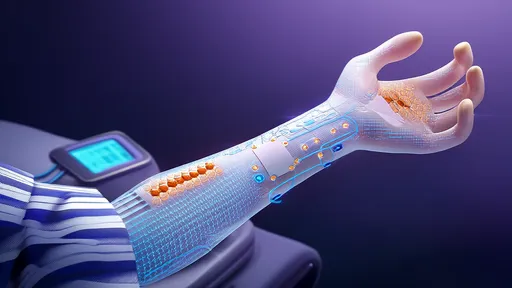
Researchers have developed a groundbreaking "smart bandage" capable of continuously monitoring key metabolic markers in sweat to provide real-time diabetes management. This wearable diagnostic technology represents a significant leap forward in non-invasive glucose monitoring and metabolic tracking.
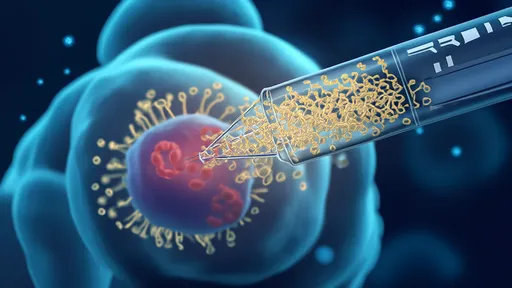
The innovative patch, created by a team of engineers and medical researchers, uses microfluidic technology to analyze sweat composition throughout the day. Unlike traditional finger-prick tests that provide momentary snapshots of blood sugar levels, this flexible electronic device offers continuous metabolic monitoring without breaking the skin.
How the Smart Bandage Works
The bandage contains an array of tiny sensors that measure glucose concentration in sweat along with other biomarkers like pH levels and lactate. These measurements correlate strongly with blood glucose levels while providing additional metabolic context. The device uses color-changing chemical indicators that can be read by smartphone cameras or dedicated optical readers.
Advanced microfluidics within the bandage ensure proper sweat collection and routing to the various sensor chambers. A unique capillary system prevents evaporation and maintains sample integrity for accurate readings over extended wear periods. The entire system is embedded in a soft, stretchable material that conforms comfortably to skin.
Clinical Significance for Diabetes Management
For the estimated 422 million diabetes patients worldwide, this technology could revolutionize daily disease management. Current monitoring methods require painful finger sticks multiple times daily or expensive implanted continuous glucose monitors. The smart bandage offers a pain-free, affordable alternative that provides similar data quality.
Perhaps most importantly, the continuous nature of the monitoring helps identify dangerous glucose spikes and crashes that might be missed with periodic testing. The additional metabolic markers give clinicians a more complete picture of patient health and treatment effectiveness.
Technical Breakthroughs Enabling the Technology
Several key innovations made this sweat-based monitoring system possible. New biosensor materials maintain stability and accuracy when exposed to sweat's complex chemical environment. Advanced hydrophilic polymers ensure consistent fluid wicking even during low-sweat conditions. Machine learning algorithms compensate for individual variations in sweat chemistry.
The research team solved previous challenges with sweat-based monitoring by developing calibration methods that account for changing sweat rates and skin temperature fluctuations. Their patent-pending reference electrode system maintains measurement accuracy over 24+ hours of continuous use.
User Experience and Practical Applications
Early prototypes have been tested on both type 1 and type 2 diabetes patients with promising results. Users report the bandage feels similar to wearing a large adhesive bandage with no discomfort. The current version provides data every 5-15 minutes, with future iterations aiming for true real-time monitoring.
The technology could be particularly valuable for pediatric diabetes patients who often struggle with frequent finger pricks. Elderly patients and those with dexterity challenges would also benefit from the automated monitoring system. Athletes and fitness enthusiasts may find the additional metabolic data useful for performance optimization.
Future Development and Commercialization
The research team is working to shrink the technology while adding more sensors to measure additional biomarkers. Upcoming versions may monitor medication levels, stress hormones, or electrolytes. Integration with existing diabetes management apps and insulin pumps is another development priority.
Several medical device companies have expressed interest in licensing the technology, with clinical trials expected to begin within two years. The inventors estimate the disposable bandages could cost between $2-5 per day - comparable to current glucose test strip expenses but providing far more comprehensive data.
Broader Implications for Healthcare
This innovation represents part of a larger trend toward wearable medical diagnostics. Similar sweat-analysis technologies are being developed for monitoring kidney function, detecting dehydration, and screening for certain cancers. The platform could eventually replace multiple blood tests with continuous, non-invasive monitoring.
The smart bandage also enables telemedicine applications, allowing doctors to remotely monitor patients' metabolic health. This could be particularly valuable for rural patients or those in developing nations with limited healthcare access. The data could help personalize treatment plans and identify needed interventions earlier.
Scientific Validation and Accuracy
Published clinical studies show the sweat-based measurements correlate strongly with blood glucose levels (r=0.89) across diverse patient populations. The system maintains accuracy during exercise, sleep, and normal daily activities. Ongoing research aims to further improve precision and expand the measurable biomarker panel.
Notably, the technology doesn't require induced sweating or physical activity to generate readings. Passive sweat production provides sufficient fluid for analysis in most environments. The sensors can detect meaningful trends even with minimal sweat volume through advanced signal processing techniques.
Comparison to Existing Technologies
Unlike continuous glucose monitors that require needle insertion, the smart bandage is completely non-invasive. It avoids the skin irritation issues common with current wearable sensors while providing additional metabolic data beyond just glucose levels. The optical readout system eliminates the need for electronic components to touch the skin.
Traditional HbA1c blood tests provide long-term glucose averages but lack the dynamic information needed for daily treatment adjustments. The smart bandage bridges this gap by offering both immediate feedback and long-term trend analysis through continuous data collection.
Regulatory Pathway and Safety
The developers are pursuing FDA clearance through the 510(k) pathway as a Class II medical device. Preliminary biocompatibility testing shows no skin irritation or allergic reactions in extended wear trials. The materials meet all standard requirements for medical adhesives and wearable devices.
Data security is another key consideration, as the system will need HIPAA-compliant wireless transmission capabilities. The team has implemented military-grade encryption for all health data transmission and storage in their prototype systems.
Potential Limitations and Challenges
While promising, the technology does face some limitations. Extreme environments (very cold/dry or hot/humid) may affect performance. Certain skin conditions could interfere with sweat collection. The researchers note that critical treatment decisions should still be confirmed with traditional blood tests until further validation is complete.
User adoption represents another challenge - some patients may need education about the reliability of sweat-based measurements. The team is developing training materials and clinician guidelines to support proper use and data interpretation when the product launches.
The Road Ahead for Metabolic Monitoring
This smart bandage technology could fundamentally change how we monitor chronic metabolic conditions. Future iterations might incorporate drug delivery capabilities, creating closed-loop systems that both monitor and treat diabetes automatically. The platform's flexibility allows for continuous upgrades as new biomarkers are validated.
As the technology matures, we may see these devices become standard tools for preventive healthcare - detecting metabolic abnormalities before symptoms appear. The convergence of wearable sensors, microfluidics, and mobile health technology promises to make personalized, proactive medicine a practical reality for millions worldwide.

By /Jul 22, 2025
By /Jul 22, 2025

By /Jul 22, 2025
By /Jul 22, 2025
By /Jul 22, 2025

By /Jul 22, 2025

By /Jul 22, 2025
By /Jul 22, 2025
By /Jul 22, 2025
By /Jul 22, 2025

By /Jul 22, 2025

By /Jul 22, 2025

By /Jul 22, 2025
By /Jul 22, 2025
By /Jul 22, 2025
By /Jul 22, 2025

By /Jul 22, 2025
By /Jul 22, 2025